Haemorrhoids Treatments
Treatment of Hemorrhoids:
Depends on Grade and severity of hemorrhoids
If only bleed only
- They are early i.e.: Grade 1 and 2
- Conservative medical, life style modification
- Rubber band ligation
If prolapse and bleed
- They are advanced i.e. Grade 2,3 and 4
- Surgical treatment
Life style advice
Eat high-fibre foods.
- Avoid food and medication causing diarrheal or constipation
- Eat more fruits, vegetables and whole grains. Doing so softens the stool and increases its bulk, which will help you avoid the straining that can cause haemorrhoids. Add fibre to your diet slowly to avoid problems with gas.
Drink plenty of fluids.
- Should drink approximately 6 to 8 (12 oz) glasses of fluid daily.
Fibre supplements.
- Fiber intake should be increased to 25 to 30 grams per day psyllium or hydrophilic colloid are often required
- Most people don't get enough of the recommended amount of fibre — 20 to 30 grams a day — in their diet. Studies have shown that over-the-counter fibre supplements, such as psyllium (Metamucil) or methylcellulose (Citrucel), improve overall symptoms and bleeding from haemorrhoids.
If you use fibre supplements, be sure to drink at least eight glasses of water or other fluids every day. Otherwise, the supplements can cause or worsen constipation.
No straining at defecation.
- Straining and holding your breath when trying to pass a stool creates greater pressure in the veins in the lower rectum.
- Squatting position is better with hip flexed at 30 degrees. This can be achieved by slightly lower toilets or placing a stool under feet while sitting on toilet.
Avoid delaying urge to open bowels.
- If you wait to pass a bowel movement and the urge goes away, your stool could dry out and be harder to pass.
Regular exercise.
- Stay active to help prevent constipation and to reduce pressure on veins, which can occur with long periods of standing orsitting.
- Exercise can also help you lose excess weight that might be contributing to your haemorrhoids.
- Walking daily up till 30 minutes /day is a good start. This helps with bowels to move and stay active
Avoid long periods of sitting.
- Sitting too long, particularly on the toilet, can increase the pressure on the veins in the anus.
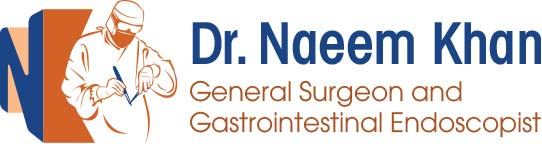
Rubber Band Ligation of Haemorrhoids
- More effective grade 2 and early grade 3 internal haemorrhoids
- May be followed by pain for up to48 h but Infection and life-threatening hemorrhage uncommon risks
It is more successful than sclerotherapy for the treatment of hemorrhoids and is well-tolerated procedure
The complication rate of rubber band ligation is less
Minor bleeding and vasovagal reaction can occur immediately after the procedure
If patient experiences pain – band has been applied too low and may need to be removed
Pain developing in 1 – 2 days may be due to ischemia
Relief with analgesia and metronidazole

Surgical Treatment
- Standard Haemorrhoidectomy
- Staple Haemorrhoidectomy
- Ligasure Haemorrhoidectomy
- HALRAR
Surgical treatment for grade III and IV hemorrhoids and is superior to any proposed conservative procedure
But pain is an issue esp.
- Post-operative pain
- Pain on defecation
- Prolonged sphincter spasm
Ligasure Haemorrhoidectomy
Ligasure is a new energy device that uses precisely calculated and focused energy deliveryto achieve the desired tissue effect.
It uses minimal amount of energy to cut tissue,resulting in less collateral damage to surrounding tissues and it cuts and coagulates and seal tissue at the same time,


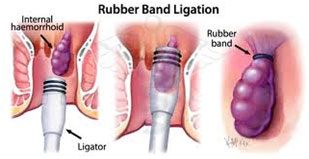
Staple Haemorrhoidectomy
Circular stapling device resects a strip of mucosa from above the dentate line It has significant reduction in post-operative pain and is faster procedure
BUT---------
- Treats only internal haemorrhoids
- Can have Serious complications
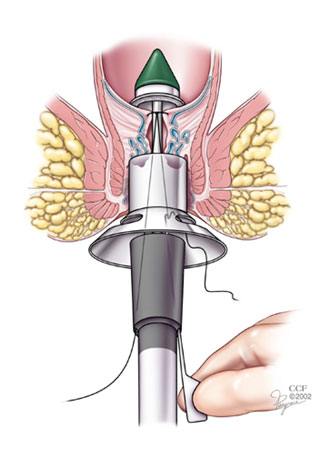
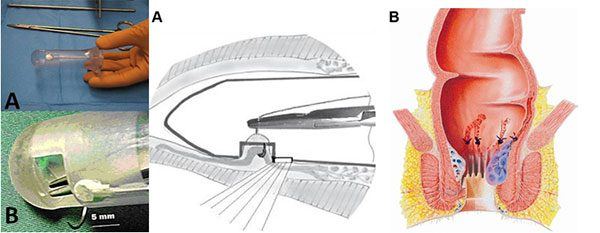
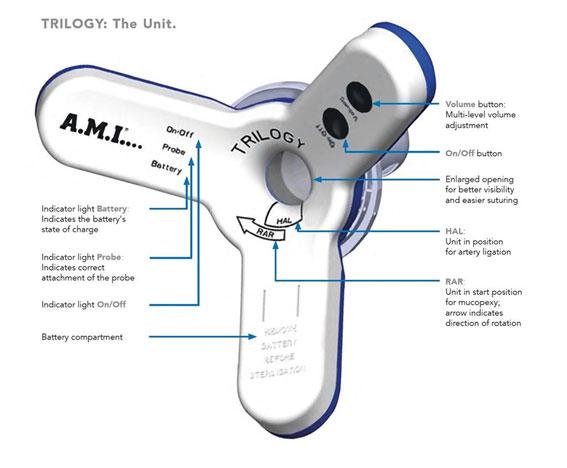
HALRAR
Doppler ultrasound probe to identify terminal branches of superior haemorrhoidal artery which are suture ligated through a slit proctoscope
This is Suture only haemorrhoidectomy and no resection is performed.
It is mini-invasive, with low morbidity, and satisfactory short- and medium-term functional results
The instrument used consists of an HALTM probe, a transparent resectoscope, provided with a centimetre-sized window at its end through which the ligations are performed. Resectoscope has light source.
A Doppler transducer, connected to the hand-held Doppler apparatus, is found at the base of this window
How can you care for yourself at home after your procedure?
Right after the procedure
Please do not drive for 24 hours after being under general anaesthesia, it may affect your judgement for 24 hours. We recommend not making any important decisions for this period of time. You are not allowed to drink alcohol, smoke, or take illicit drugs for at least 24 hours.
Pain relief:
Local anaesthetic will be provided for pain relief after the procedure but this will wear off over the next few hours. It is important to take some painkillers before the pain becomes intense, as it will then be harder to control. You should use Panadol 1 gram every six hours and Ibuprofen 400 milligrams every eight hours for the next 48 hours. You should check with your doctor that it is appropriate for you to take Ibuprofen.
If you require stronger pain relief Endone 5 milligram may be used but this will require a prescription. (- You may feel nausea and constipation. If the nausea is affecting you a lot, stop the medication or speak to your doctor. If you are experiencing constipation, you may take Lactulose to avoid straining.) You must not drive or work while using this medication.
*If you have any allergic reaction, please stop taking the medication and call 000 immediately.
Salt Baths
Warm baths are quite soothing when you are in pain. A 1-2 tablespoonful of cooking salts may be added to the bathwater in order to help keep the wound clean. If you find it helpful you can bath 2–3 times per day and after bowel movements.
Bowel Movements
Your bowels will continue to work normally after your surgery. It is best to avoid becoming constipated, as hard motions will increase you level of discomfort. Use of lactulose 20 mls twice a day is recommended. But Metamucil one teaspoon twice daily may be used for the first week after surgery. It is normal to experience pain with bowel movements for the first week or so after surgery. You may see blood on the toilet paper or in then bowl with the first few bowel motions.
Wound care
Operative wound in this area takes longer to heal because of continuous movement and contamination with the stools. Small amount of bleeding and discharge from the raw operative area is also common. it is not unusual for the operative area to swell up for few days because of the surgical trauma to the area. Use water showers to clean the area after opening the bowels. You can also use baby wipes if water showers are not available.
- Put ice on your anal area several times a day for 10 minutes at a time. Put a thin cloth between the ice and your skin. Follow this by placing a warm, wet towel on the area for another 10 to 20 minutes.
- Keep the anal area clean, but be gentle. Use water and a fragrance-free soap, such as ivory, or use baby wipes or medicated pads, such as tucks.
- Wear cotton underwear and loose clothing to decrease moisture in the anal area.
- Nearly every patient will have bloody drainage or a small amount of bleeding after the procedure and this may last for a few weeks. If the bleeding doesn’t stop for more than 20 mins, please call our office or 000 immediately.
Recovery & post operative care
- Eat more fibre. Include foods such as whole-grain breads and cereals, raw vegetables, raw and dried fruits, and beans.
- Aim to drink 1.5 to 2L of water every day
- It is important to avoid constipation after the procedure. Use a stool softener that contains bran or psyllium. You can save money by buying bran or psyllium (available in bulk at most health food stores) and sprinkling it on foods and stirring it into fruit juice. Or you can use a product such as Metamucil or Hydrocil.
- Practice healthy bowel habits. Go to the bathroom as soon as you have the urge. Avoid straining to pass stools. Relax and give yourself time to let things happen naturally. Do not hold your breath while passing stools. Do not read while sitting on the toilet. Get off the toilet as soon as you have finished.
- You may feel like you have to have a bowel movement without any stool actually being present in your rectum. This feeling may frequently follow hemorrhoidectomy and may last for up to a month.
- It is important to have a follow up appointment with the surgeon in 1 weeks.
Reflags to watchout
Small amount of bleeding and discharge is not uncommon after the surgery.
But you should notify your doctor immediately or call an ambulance as soon as practicable. to go the emergency department of public or private hospital if you have following symptoms;
- Feel unwell with high fevers and shivers,
- Passing large volume bleeding and blood clots,
- Difficulty passing urine or increasing pain,
Returning to routine activities
This is unfortunately a painful procedure so you will need 5–14 days off work. Sport and vigorous physical activities should be avoided for 2–3 weeks.