Hernia Surgery
How is an inguinal hernia treated?
Most people will be advised to have surgery as this will reduce the main problem with an inguinal hernia — the hernia might trap the part of the bowel that is poking through the defect or weak part of abdominal wall
Surgery is the only treatment for hernia and watchful waiting is usually not recommended but can be an option if have no symptoms or any complications and if patient is high anaesthetic risk.
- Open technique;
A tension-free open mesh repair is the gold-standard for the treatment of an inguinal hernia. It has been associated with low recurrence rates, can be performed under local anaesthesia, and does not require specialized training or equipment - Laparoscopic technique
Through a small incision (Key -hole) and insertion of ports where a camera and different instruments are inserted
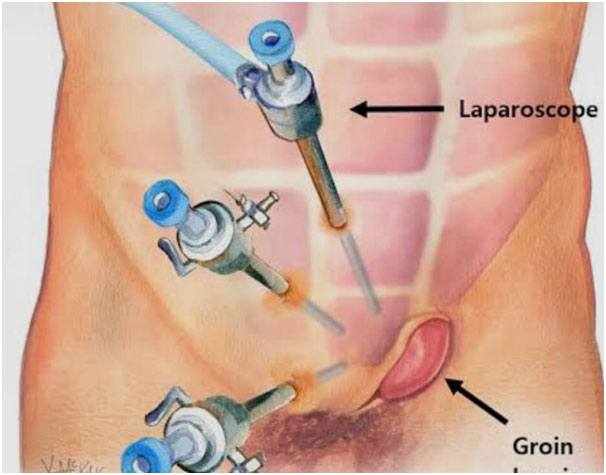
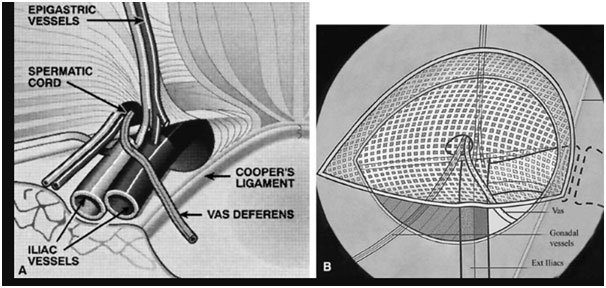
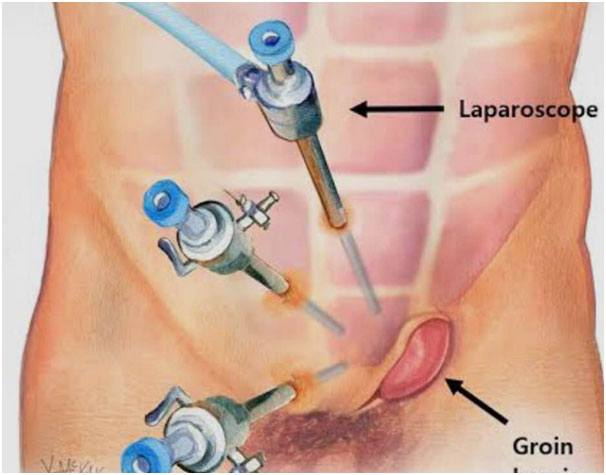
Laparoscopic or Conventional Inguinal Herniorrhaphy
Most comparative trials have shown equivalent recurrence rates between open and laparoscopic mesh repair with following advantages of laparoscopic over open technique;
- Less acute and chronic pain
- Earlier return to work
- Less infection
- Fewer wound complications
- Less numbness
- Faster in bilateral repairs
- Recommended in recurrent hernias
Contraindications of laparoscopic surgery;
- The inability to tolerate general anaesthesia for any reason and
- hostile abdomen are clear contraindications to laparoscopic hernia repair.
- Surgeons must carefully evaluate their patients to ensure that laparoscopic technology is properly applied
What is a Surgical Mesh and why surgeons use a mesh?
There is very strong evidence to suggest that tension free repair of the hernia defect using a surgical mesh reduces the risk of hernia recurrence.Hernia mesh is used in more than 90% of the surgical repairs
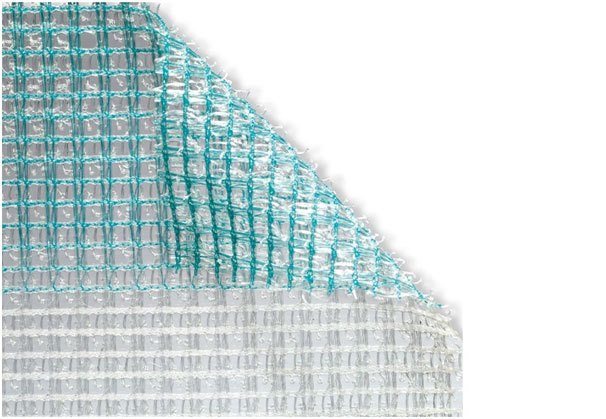
Surgical mesh is a medical device that supports the damaged tissue while inducing the scar formation. There are small pores in the mesh that allow the granulation tissue to grow and mesh acts as a skeleton for the scar tissue to form eventually leading to the incorporation of mesh in the scar tissue leading to a strong repair.
There is general tendency to use light meshes with macropores which reduce the post-operative risk of chronic pain and mesh infection.

What are the types of surgical mesh?
There are two main broad categories of meshes being used currently;
Absorbable Mesh:
They are also called biological meshes. These meshes tend to degrade and lose strength over time. During the process of the degradation, surgical mesh induces tissue growth and provides strength to the repair.
Most of the biological meshes are manufactured from animal tissue using intestine or skin of pig or cow.
Absorbable mesh is suitable option for patients where there is tissue contamination and a risk of infection.
Non-absorbable Mesh:
They remain in body indefinitely and considered as permanent implants
They’re not degrading and they induce scar growth into the tissues and provide a strong repair. The commonest non-absorbable mesh being used world-wide is poly propylene.
There is a small risk associated with the use of mesh in surgical repair such as pain especially within first 2 weeks, mesh infection and bowel obstruction due to adhesions of mesh to bowels.
Postoperative care
- Most of patients can be discharged on day of surgery.
- Early mobilisation is encouraged as soon as possible after the surgical procedure.
- Avoid any heavy lifting more than 5-7 KG for a period of 6-8 weeks is recommended
- Postoperative pain relief is usually in the form of oral simple analgesic with combination of short acting opiates for breakthrough pain. Few require analgesia after 48 hours.
- Most patients can return to light duties after 2 weeks avoiding any heavy lifting more than 7 kg, and no bending, pushing, pulling, squatting, twisting and lifting above shoulders for 6 weeks period. They can resume normal duties including heavy lifting after 8 weeks.
- Daily walking programme on the first postoperative day, progressively increasing the distance walked.
- Driving is permissible when the patient feels legally able to do so - usually judged by the ability to perform a simulated emergency stop without discomfort. This is usually after 5-7 days.
Some postoperative problems
- Skin anaesthesia: This is normal after this procedure. Patients should be told that this will progressively return to normal over several months.
- Skin bruising and haematoma: Patients can be reassured that bruising of the inguinal and scrotal skin is painless and self-limiting.
- Seroma: Formation of seroma can probably be reduced by limiting dissection
- Pain: Apart from acute post-operative pain, there is small group of patients developing chronic pain which last beyond 3 months.
- Ischaemic orchitis and testicular atrophy: very small risk only.
- Recurrence: Hernia recurrence can be minimised by using a large size of mesh (15 x 10cm) with minimal trimming.
Apart from skin anaesthesia the majority of patients have no such problems.