Hernia
Hernia-Types and Management
Definition
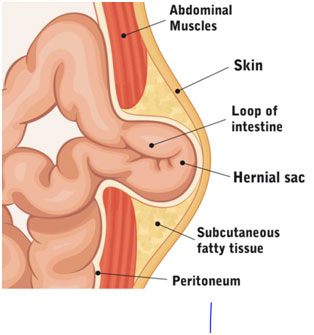
A hernia is a medical condition which occurs when fatty tissue or an organ pushes through weakness in the muscle wall or connective tissue of the containing cavity.
Groin herniorrhaphy is the most common operation performed by general surgeons.
Epidemiology
Hernia repair surgery is considered to be the world’s most common surgical procedure.
Annually, more than 20 million groin hernias are repaired worldwide.
Why Surgical repair is recommended
The general approach towards groin hernias is surgical repair regardless of the presence of symptoms. Hernias usually don’t get better on their own and they tend to get bigger making surgical procedure more difficult with increased risk of surgical complications
The doctors usually recommend hernia surgery because of the following symptoms:
- Risk of incarceration of the hernia contents -The tissue becomes trapped in the abdominal wall. That’s when the blood supply to the tissue gets cut off.
- Risk of strangulation of the hernia contents; The hernia becomes strangulated. This can cause permanent damage and is a surgical emergency.
- Pain and discomfort-The hernia causes pain or discomfort, or it’s growing larger.
A surgical hernia repair involves pushing the bulge back inside the body part that should contain it and keeping it there.
History of hernia repair
The history of hernia repair is the history of surgery
The Egyptian Papyrus of Ebers (circa 1552 Ac) contains an observation on hernias:
when you judge a swelling on the surface of a belly, what comes out,caused by coughing
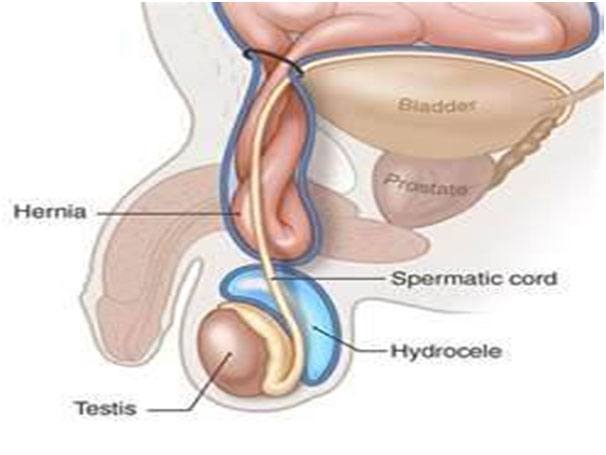
Ancient Greeks (Hippocrates, 400 BC) differentiated between hernia and hydrocele Taxis was recommended for strangulation
The history of open surgery for groin hernia has gone through many stages of Development as below:
- The ancient era (ancient times to the fifteenth century)
- The era of the start of Herniology (fifteenth to seventeenth centuries)
- The anatomic era (seventeenth to nineteenth centuries)
- The era of repair under tension (nineteenth to mid-twentieth century)
- The era of tensionless repair mid-twentieth century to the present,
Despite the introduction of anesthesia in 1846, surgery on hernias made little progress during the first half of the nineteenth century, as any attempt to open the inguinal canal was followed by severe sepsis and recurrence of the hernia.
Lister introduced antiseptic carbolic spray to surgery about 1870.
When Von Mickulicz translated antiseptic surgery to aseptic surgery in 1904, the scene was set for the techniques of modern hernia surgery to develop.
What are the symptoms of hernia?
The symptoms of a hernia depend on the size of the hernia and where it is.
Typical symptomsinclude:
- A bulge or lump in the groin or abdomen
- Pain, burning, aching, heaviness or discomfort, especially when coughing, straining or lifting
- A pulling sensation around the lump or bulge
Some hernia may not cause any symptoms.
Hernia can present as an emergency with following symptoms
- A bulge that is painful and hard
- A bulge that looks red, purple or dark
- A bulge that doesn’t change in size or reduce size when straining
- Redness and tenderness at the site
What are types of hernia
- Inguinal 75%
- Umbilical 15%
- Femoral 5%
- Miscellaneous other types count for the rest 5-10%
Inguinal Hernia
Accounting for 75% of all abdominal wall hernias, and with a lifetime risk of 27% inmen and 3% in women, inguinal hernia repair is one of the most commonlyperformed surgeries in the world.
In the United States inguinal herniorrhaphy accounts for approximately 800,000cases year
It was in February 1989when Lichtenstein and associates reported on 1000consecutive patients with primary repair of inguinal hernia usingtension-free repair employing a Marlex mesh prosthesis to bridgethe direct floor of the groin without approximating the tissue defect.
Polyester mesh was the first popular non-metallic mesh to stand thetest of time. It is mainly replaced with polypropylene mesh
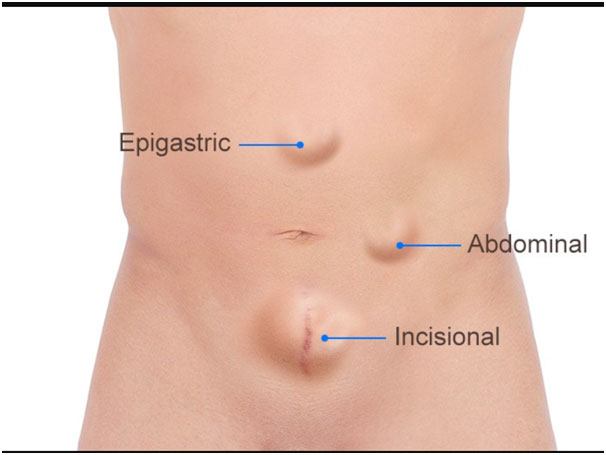
Umbilical and para-umbilical hernia
- Umbilical Hernia
Prevalence in the adult population is 2%
Adult umbilical hernias have an acquired origin as a consequence of increases in pressure (pregnancy, ascites, etc.), the pull of the abdominal muscles, and the deterioration of connective tissue. - Para-umbilical hernia;
Para-umbilical hernia is due to disruption of linea alba above the umbilical cicatrix and usually occurs in elderly patient with connective tissue degeneration and patients with a chronic cough.
The high morbidity and mortality associated with incarcerated umbilical hernias demand an elective repair in all circumstances.
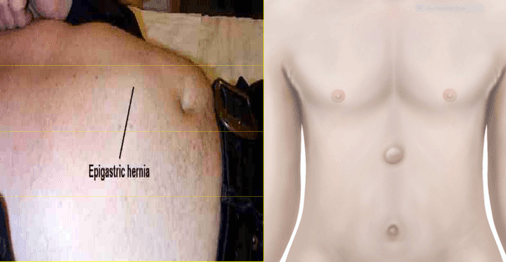
Epigastric Hernia
Occur in the linea alba between the xiphoid process and the umbilicus
Small defects (< 1cm). Usually contains pre-peritoneal fat and may become quite tender Defect closed by dissection of the ring and direct closure.
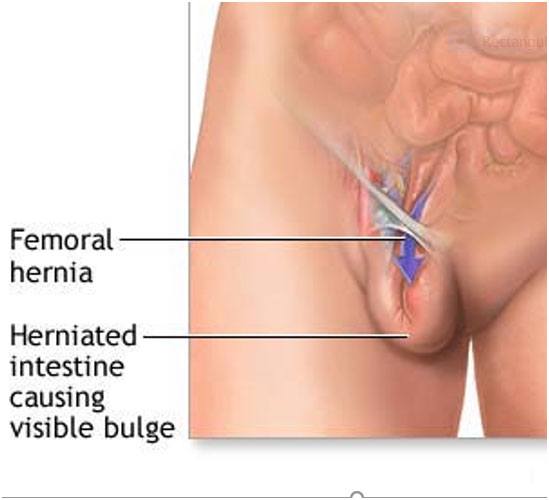
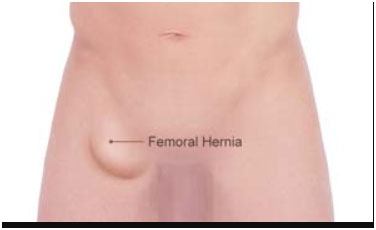
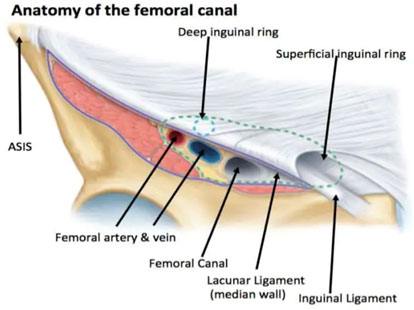
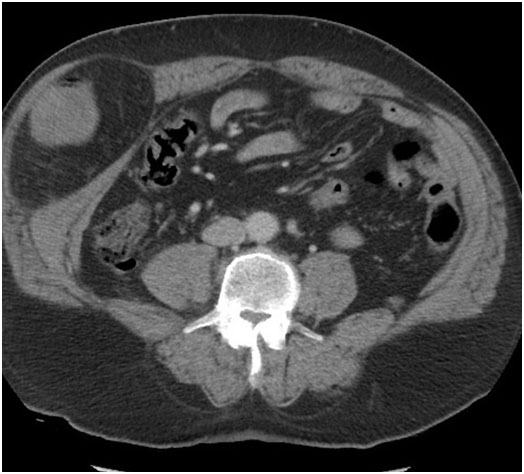
Femoral hernia
3rd most common hernia-20% in women and 5% men
Present with Strangulation in 40 % of times
Females have 4x higher incidence. Most common in middle-aged and elderly women
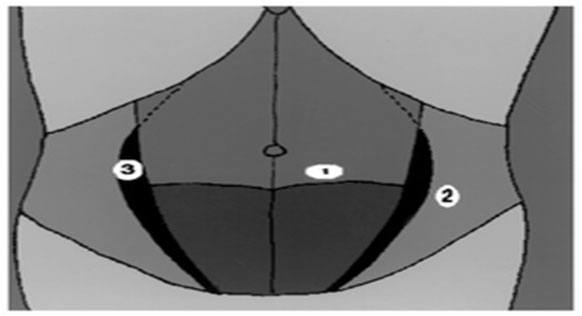
Spigelian hernia
Rare partial abdominal wall defect that occurs through a defect in the transversus abdominis aponeurosis (Spigelian fascia).
Named after Belgian anatomist Adriaan van den Spieghel.
Hernia most commonly presents at the level of the semicircular line (arcuate line of Douglas) – below this the aponeurosis is a single layer and resistant to herniation.
Overlying external oblique muscle and fascia remain intact.
Late diagnosis and tends to present as an emergency.
- Semicircular line
- Linea semilunaris
- Spigelian fascia
Incisional hernia
Hernial formation through failure of healing of previous surgically created fascial defect. Common causes are;
- Iatrogenic
- Multifactorial local and systemic factors
- Old age, pulmonary disease, malignancy, obesity
Incidence
10% of all anterior abdominal wall incisions.
More common following midline incisions through avascular linea alba (11- 20%)
May present with
- Incarceration (6 – 15%)
- Strangulation of bowel (2%)
- Intestinal obstruction
May cause intermittent pain

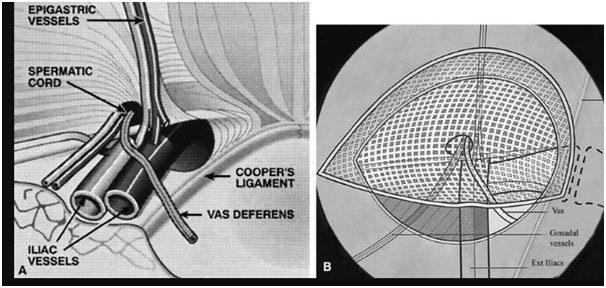
How is an inguinal hernia treated?
Most people will be advised to have surgery as this will reduce the main problem with an inguinal hernia — the hernia might trap the part of the bowel that is poking through the defect or weak part of abdominal wall
Surgery is the only treatment for hernia and watchfulwaiting is usually not recommended but canbe an option if have no symptoms or any complications and if patient is high anaesthetic risk.
- Open technique;
A tension-free open mesh repair is the gold-standard for the treatment of an inguinal hernia. It has been associated with low recurrence rates, can be performed under local anaesthesia, and does not require specialized training or equipment - Laparoscopic technique
Through a small incision (Key -hole) and insertion of ports where a camera and different instruments are inserted
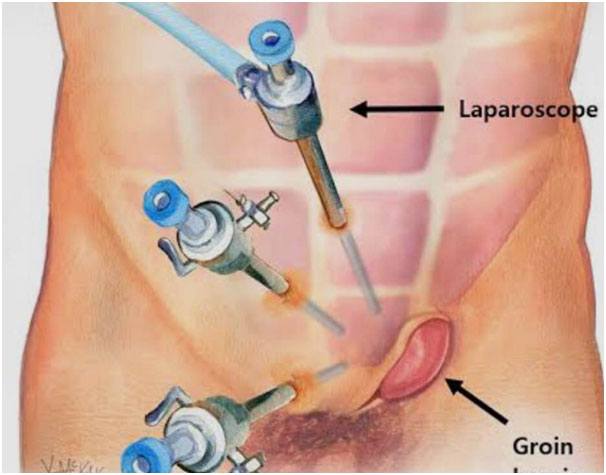
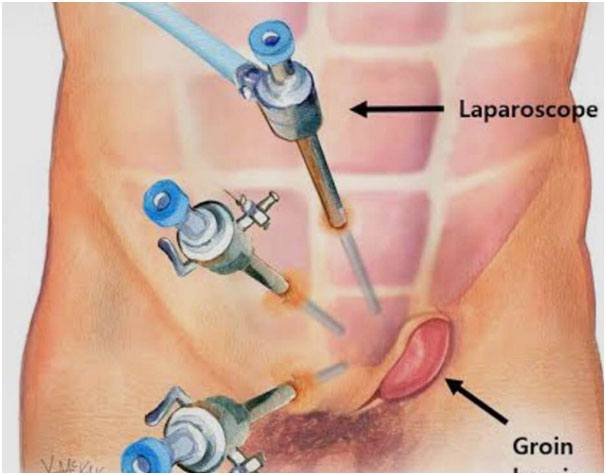
Laparoscopic or Conventional Inguinal Herniorrhaphy
Most comparative trials have shown equivalent recurrence rates between open and laparoscopic mesh repair with following advantages of laparoscopic over open technique;
- Less acute and chronic pain
- Earlier return to work
- Less infection
- Fewer wound complications
- Less numbness
- Faster in bilateral repairs
- Recommended in recurrent hernias
Contraindications of laparoscopic surgery;
- The inability to tolerate general anaesthesia for any reason and
- hostile abdomen are clear contraindications to laparoscopic hernia repair.
- Surgeons must carefully evaluate their patients to ensure that laparoscopic technology is properly applied
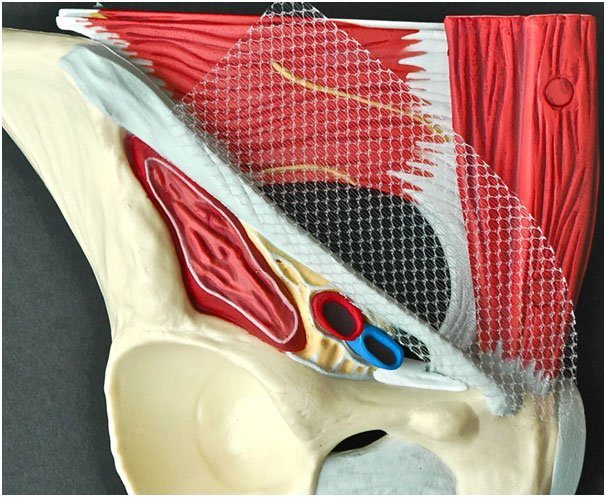
What is a Surgical Mesh and why surgeons use a mesh?
There is very strong evidence to suggest that tension free repair of the hernia defect using a surgical mesh reduces the risk of hernia recurrence.Hernia mesh is used in more than 90% of the surgical repairs
Surgical mesh is a medical device that supports the damaged tissue while inducing the scar formation.There are small pores in the mesh that allow the granulation tissue to grow and mesh acts as a skeleton for the scar tissue to form eventually leading to the incorporation of mesh in the scar tissue leading to a strong repair.
There is general tendency to use light meshes with macropores which reduce the post-operative risk of chronic pain and mesh infection.
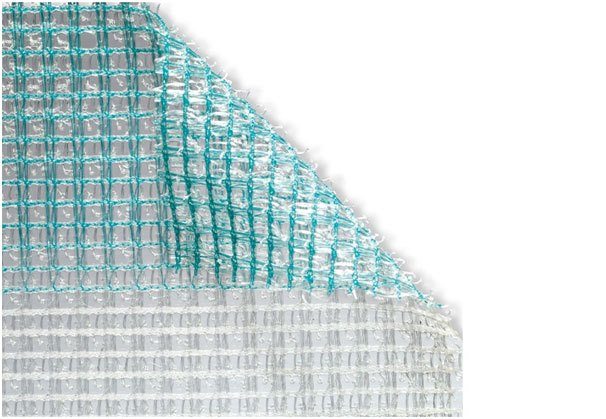

What are the types of surgical mesh?
There are two mainbroad categories of meshes being used currently;
Absorbable Mesh:
They are also called biological meshes. These meshes tend to degrade and lose strength over time. During the process of the degradation,surgical meshinduces tissue growth and provides strength to the repair.
Most of the biological meshes are manufactured from animal tissue using intestine or skinof pig or cow.
Absorbable mesh is suitable option for patients where there is tissue contamination and a risk of infection.
Non-absorbableMesh:
They remain in body indefinitely and considered as permanent implants
They’re not degrading and they induce scar growth into the tissues and provide a strongrepair. The commonest non-absorbable mesh being used world-wide is poly propylene.
There is a small risk associated with the use of mesh in surgical repair such as pain especially within first 2 weeks, mesh infection and bowel obstruction due to adhesions of mesh to bowels.
Postoperative care
- Most of patients can be discharged on day of surgery.
- Early mobilisation is encouraged as soon as possible after the surgical procedure.
- Avoid any heavy lifting more than 5-7 KG for a period of 6-8 weeks is recommended
- Postoperative pain relief isusually in the form of oral simple analgesic with combination of short acting opiates for breakthrough pain. Few require analgesia after 48 hours.
- Most patients can return to light duties after 2 weeks avoiding any heavy lifting more than 7 kg, and no bending, pushing, pulling, squatting, twisting and lifting above shoulders for 6 weeks period. They can resume normal duties including heavy lifting after 8 weeks.
- Daily walking programme on the first postoperative day, progressively increasing the distance walked.
- Driving is permissible when the patient feels legally able to do so - usually judged by the ability to perform a simulated emergency stop without discomfort. This is usually after 5-7 days.
Some postoperative problems
- Skin anaesthesia: This is normal after this procedure. Patients should be told that this will progressively return to normal over several months.
- Skin bruising and haematoma: Patients can be reassured that bruising of the inguinal and scrotal skin is painless and self-limiting.
- Seroma: Formation of seroma can probably be reduced by limiting dissection
- Pain:Apart from acute post-operative pain, there is small group of patients developing chronic pain which last beyond 3 months.
- Ischaemic orchitis and testicular atrophy: very small risk only.
- Recurrence: Hernia recurrence can be minimised by using a large size of mesh (15 x 10cm) with minimal trimming.
Apart from skin anaesthesia the majority of patients have no such problems.