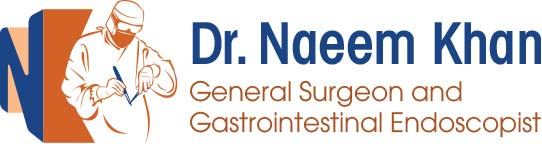
Anal Fissure
Definition:
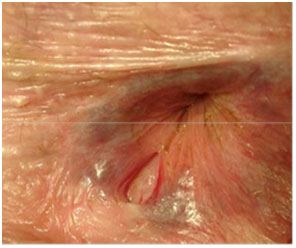
- Ulcer or split in the skin lined (distal) part of the anal canal.
- Classical symptom is stab like / cutting glass pain on defecation
- Most fissure are acute and heal spontaneously.
- Common site is posterior midline (women-10% anterior)
Common Causes:
- Constipation-hard faecal bolus
- Childbirth(3-10%)
- Crohn’s disease -Management is medical- Immunosuppressives, Antibiotics, Little role for surgical treatment
- Occasional diarrheal especially in children
- Anal SCC
- Post-operative – haemorrhoidectomy
Chronic fissure;
- (Fissure becomes chronic when it fails to heal for >6 weeks)- Thick indurated edges
- Sentinel tag
- Absence of granulation tissue with white fibres of Internal Anal Sphincter (IAS) visible at base.
- There is associated spasm of IAS causing pain and discomfort

Spasm of internal sphincter
- Leading cause of non-healing is spasm of the internal anal sphincter
- Poor blood supply and perfusion –posterior midline ischemia
- Treatment (both medical and surgical) is aimed at restoring the normal tone of the IAS

Treatment
- Medical /Non-operative treatment
- Stool softeners
- Sitz baths
- Topical anaesthetics 2 % Lignocaine Jelly
- Anti-inflammatory ointment
- Pharmaceutical Treatment
- Topical Nitroglycerin GTN(nitric oxide) -Rectogesic 0.2% ointment
- Topical calcium channel blockers
- Oral calcium channel blockers
- Botulinum toxin injections
- Surgical treatment
- Lateral internal sphincterotomy (LIS) -(Currently Recommended Surgical Management)
- Anal advancement flap (alternative to LIS)
- Fissurectomy
- Anal dilation (considered but not recommended
- Rectogesic ointment -GTN
- Reducing intra-anal pressure (relax IAS)
- Vasodilatory effect on anal vessels -Topical paste applied three time a day
- 0.2% strength (compared with 2% strength for GTN patches)
- >80% fissures healed in 2-3 weeks
- Side effects include headaches, flushing and dizziness on standing, burning sensation in the anus, development of tolerance.
- 25% of patients will be unable to tolerate
- Calcium channel blockers (topical) is an alternative
- 1- 2% Diltiazem cream-less S/E
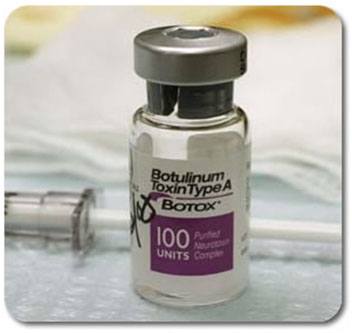
- Botulinum toxin (Botox®) injection
- Rapid action-within few hours
- Non traumatic
- Effect last 3-4 month –enough for fissure to heal
- No damage /division of IAS
- Very good option in females-already attenuated IAS
- Surgery-Lateral sphincterotomy;
- 96% healing rate
- Partial division of Internal sphincter
- S/e-30 incontinence- Females at greater risk due to anatomically shorter anal sphincter and pre-existing childbirth injury.
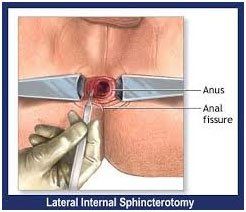
Advantages
- Can be performed under LA as a day case
- Wounds heal quickly
- Low recurrence rates
- Can perform concomitant procedure without increased risk of complication Ref; Leong, Dis Colon Rectum 1994; 37:1130-1132
Disadvantages
- Impaired continence - up to 38% notice some change
- Soiling - 27% (open) vs 16% (closed); p< 0.001
- Stool - 12% vs 3%; p< 0.001
- Flatus - 30% vs 24%; p< 0.062
Ref; Garcia-Aguilar, Dis Colon Rectum 1996; 440-443 (549 patients)
- 96% healing rate
- Lords manoeuvre;
- Forceful dilatation (8 fingers)of the sphincter complex is not practiced now days
- If fissure is not Non healing
- Consider Crohn’s disease
- HIV
- Malignancy
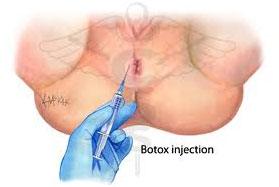
Botox VERSUS Lateral internal Sphincterotomy (LIS)
- RCT, 111 patients
- 20-30 IU Botox(R) injected anteriorly (50) vs open LIS (61)
| LIS | Botox | |||
|---|---|---|---|---|
| Healing | @ 1/12 | 82% | 74% | (p = 0.023) |
| Healing | @ 6/12 | 96% | 87% | (p = 0.212) |
| Healing | @ 12/12 | 94% | 75% | (p = 0.008) |
| Incontinence | 16% | 0% | (p < 0.001) | |
| Return to work | 15 days | 1days | (p < 0.0001) |
Mentes, Dis Colon Rectum 2003; 46:232-237